Coping amid disaster: How we can mentally prepare for a pandemic winter
This week marks six months since Washingtonians were directed to the stay at home amid the coronavirus pandemic. The changes have affected all of us.
Dr. Kira Mauseth is a practicing clinical psychologist. She sees patients at Snohomish Psychology Associates, teaches at Seattle University, and helps lead the Behavioral Health Strike Team for the Washington State Department of Health.
This interview has been edited for clarity.
I think the biggest thing for behavioral health, in the context of Covid-19, is really to recognize that nobody is immune to the experience of living through a pandemic. We're all probably being affected emotionally and behaviorally in ways that we don't really realize.
It's affecting everything, on a very small level, on our day to day interactions with our kids and with our families, and with strangers, at the grocery store, and people that we encounter, even on social media. I think it's really important to recognize that being in a disaster, and recovering from a disaster, and being part of that cycle, affects how our brains are functioning right now. That has an impact on everything.
Sponsored
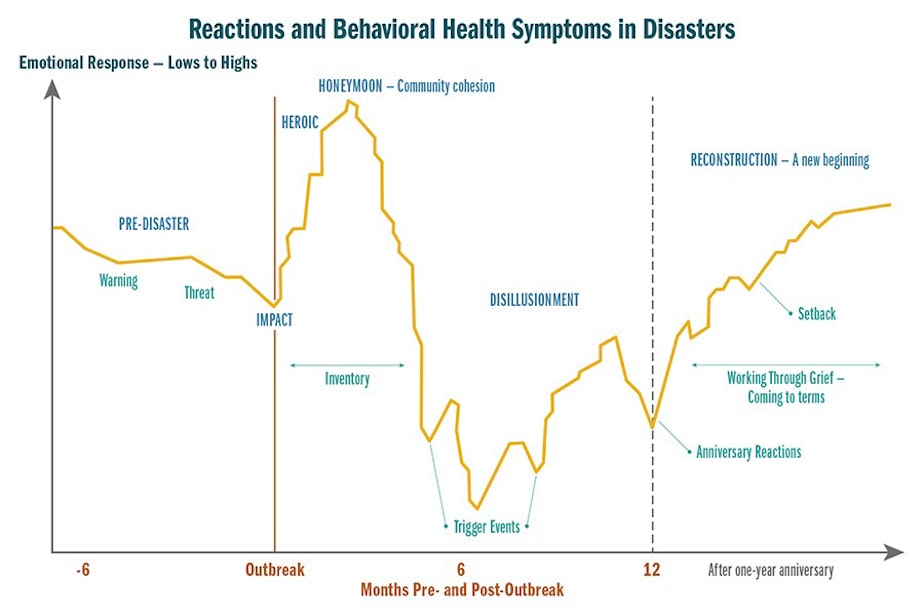
There have been a lot of disasters all over the world and nationally, and we've been able to look at disaster science and learn about how human beings respond to disaster in a fairly predictable way from a behavioral health perspective. We're using that to develop some of the forecasting and guidance that we're doing for the state right now.
I think the biggest concerns are the things that happen from an emotional response perspective. It's pretty typical and pretty normal for all of us to be behaving and be expressing ourselves a little bit more emotionally than we otherwise would. That's because the part of our brain that is responsible for emotion is a little bit more influential right now. Again, a normal part of the disaster recovery and response.
But one of the consequences of that is that we lose a little bit of our ability to take in details and sort through what we need to be reacting to, and maybe what can wait, and give ourselves that space to respond logically and calmly. Most of us are more apt to be quick to anger, and maybe easy to frustrate, and more likely to start an argument.
That's one of the things that I'm concerned about heading into the fall — the effect that that has for all of us on how we interact with each other, and then the resulting sense of either anxiety or depression that comes from feeling like you're kind of stuck in that mode.
Sponsored
[The impact on people's health] is pretty significant. Usually, with behavioral health care, there's a lull in the summer months, where people are on vacation with their families. They're generally feeling better and doing better. In private practice, we see a little bit of a downturn in August, typically. There was no such lull in 2020.
What we know is that six to nine months post-impact is when symptoms are the worst, because that's how long it takes your brain to adjust to what's happened — regardless of the type of disaster. That six to nine month window is what we're coming into right now for the fall. Again, regardless of the type of disaster. We're anticipating behavioral health needs, regardless of whether there's a second wave of illness or not, being the strongest between now and December of 2020.
The numbers of depression in the state have gone up. In June, we were close to 2 million people. We're anticipating a total of about 3 million people, out of what, seven and a half? Around 40-something percent of Washingtonians with clinically significant symptoms by the end of the year.
We really focus on identifying the aspects of resilience that you can bring to bear on your day to day life and functioning. We look at purpose, flexibility and adaptability, connection, and hope. One of the most important things folks can do is change the scope of their expectations.
Sponsored
I mean, thinking about what's motivating you to get out of bed this week, and today, not worrying about what's coming in December or what you're going to do for the holidays, yet. Just taking it really a day at a time, or a week at a time, and keeping the scale of your expectations for yourself and for other people a little bit more manageable, and smaller.
Behavioral Health Resources in Washington State
The Crisis Connections Washington Listens line is 833-681-0211
Listen to the interview by clicking the play button above.


