Coronavirus variants seem to 'evade immunity.' Here's what that really means
From beta to delta, and now omicron, terms like "evades immune response" or "escapes immunity" are commonly used to describe the potential dangers of coronavirus mutations.
It might sound as if vaccines and immunity are useless. But the reality is more nuanced, and immunity is not entirely lost. So what does "evading immunity" even mean?
Han Solo evaded Imperial TIE fighters. Bonnie and Clyde evaded the fuzz. And now variants evade immunity. That sounds like these variants are dodging vaccines and antibodies altogether, bringing us back to square one. Are they?
Not quite.
As Deborah Fuller, a microbiologist at University of Washington School of Medicine explains, the antibodies that offer us protection may lose one angle of attack, but it's not the only angle.
RELATED: Omicron was in Europe a week before South Africa reported it
"Say a new variant emerges, it mutates ... and messes up one site that antibodies can use to block an infection, there are still other antibodies out there that are going to be able to bind to other parts of the spike protein,” Fuller said.
Sponsored
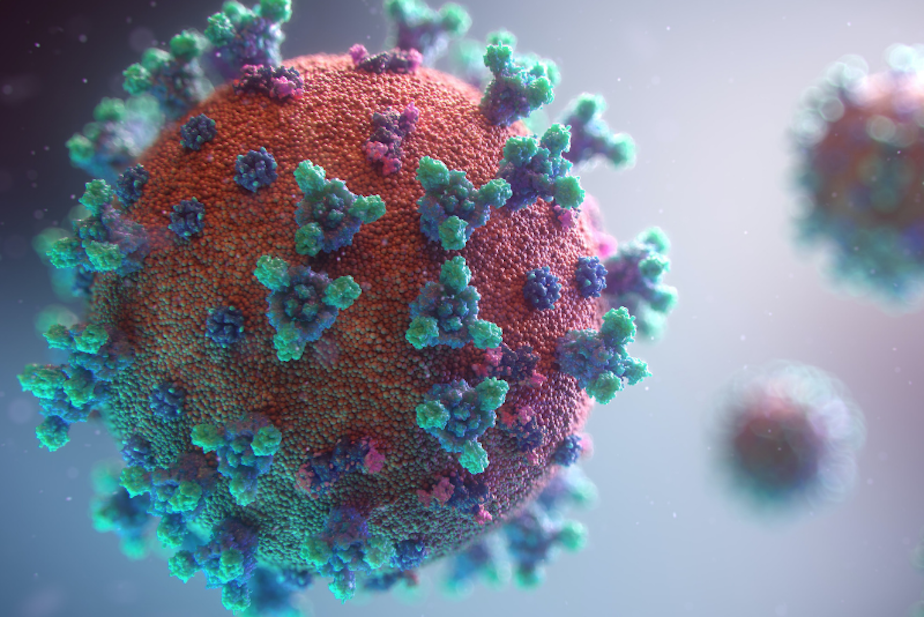
The spike protein we often hear about when talking about coronavirus is the mechanism the virus uses to infect our cells.
"The vaccines are designed to make what we call ‘polyclonal antibodies,’ which means there are antibodies that interact with the spike protein at multiple different spots — not just one."
Fuller said that some of our antibodies may "fall off" when a virus mutates. In that sense, a particular mutation "evades" or partially evades antibodies.
"And now (antibodies) can’t bind quite as effectively to the virus as they used to … but that doesn’t mean the antibodies aren’t still working," Fuller said. "They are still slowing it down and interfering with that infection, but just not as efficiently as it was when there were not mutations."
Antibodies are part of a bigger immune system at work
Sponsored
"Evade" or similar words used in this medical context should not be interpreted as if coronavirus variants are entirely getting around immunity from natural infection or vaccines (though vaccines offer more consistent protection).
Covid vaccines have mostly been designed to target the spike protein on the coronavirus. Our bodies learn to produce antibodies that interfere with the spike protein's ability to enter our cells.
We likely have antibodies for other parts of the virus, too. Other aspects of the immune system — like white blood cells called T cells, which help the body adapt an immune response — also come into play.
“(Viruses) like to evade antibodies ... they have a harder time evading those T cell responses," Fuller said.
Antibodies may be the first on the scene, but T cells arrive next. If the virus does get into a cell, T cells show up to eliminate it. This is one situation where breakthrough infections happen.
Sponsored
“We still get the breakthrough infections, but it helps us clear the infection much more quickly so we don’t end up getting the disease or severe disease," Fuller said. "And that might be why a lot of our vaccines are still holding their own against a lot of these new variants, even though they are developing these mutations.”
How a mutation affects vaccine efficacy takes time to determine. With omicron, and its many mutations, researchers will likely know within a couple weeks. They do this by testing immunized blood against the variant in a lab. Fuller notes that this initial test only measures how effective antibodies are, not other parts of the immune system like T cells. That takes a little longer to determine.
Fuller also notes that since omicron was first detected on November 24, its code was sent to the University of Washington School of Medicine and her lab has already been making vaccines for it.
“My lab is plugging it in today," she said, adding that mRNA technology will allow for such vaccines to adapt and be released within months.

