Putting A Price On COVID-19 Treatment Remdesivir
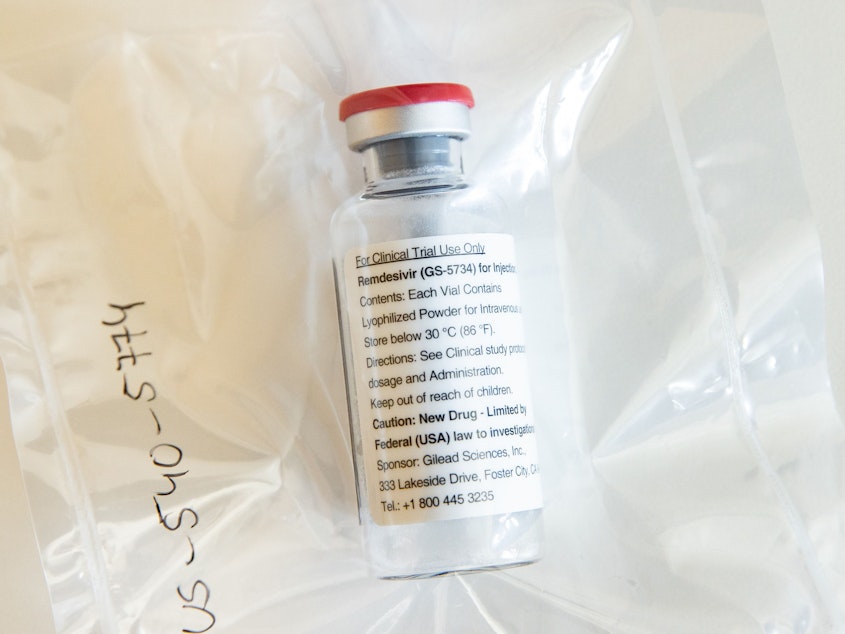
Now that the Food and Drug Administration has authorized remdesivir for emergency use in seriously ill COVID-19 patients, the experimental drug is another step closer to full approval. That's when most drugs get price tags.
Gilead Sciences, which makes remdesivir, is donating its initial supply of 1.5 million doses, but the company has signaled it will need to start charging for the drug to make production sustainable. It's unclear when that decision might be made.
"Going forward, we will develop an approach that is guided by the principles of affordability and access," Gilead CEO Daniel O'Day told shareholders during the company's annual meeting Wednesday.
In a quarterly financial filing made the same day, Gilead said its investment in remdesivir this year "could be up to $1 billion or more," much of it for scaling up manufacturing capacity.
The company also acknowledged that it's in the spotlight. "[G]iven that COVID-19 has been designated as a pandemic and represents an urgent public health crisis, we are likely to face significant public attention and scrutiny about any future business models and pricing decisions with respect to remdesivir," Gilead said in the quarterly filing.
How will the company balance its business calculations with the drug's potential value to society?
"Gilead has not yet set a price for remdesivir," company spokeswoman Sonia Choi wrote in an email to NPR. "At this time, we are focused on ensuring access to remdesivir through our donation. Post-donation, we are committed to making remdesivir both accessible and affordable to governments and patients around the world."
Among potential treatments for COVID-19, remdesivir, an intravenous drug that was once studied for Ebola, is one of the furthest along.
"It's hard to imagine a situation in which there will be more public scrutiny," said Michael Carrier, a professor at Rutgers School of Law who specializes in antitrust and pharmaceuticals. "On the one hand, Gilead will try to recover its R&D in an atmosphere in which it is able to potentially make a lot of money. On the other hand, the pressure will be intense not to charge what's viewed as too high a price."
Breaking with its usual practices, the Institute for Clinical and Economic Review, or ICER, an influential nonprofit that analyzes drug pricing, issued an expedited report on remdesivir.
"Under normal circumstances, we would be unlikely to do a report when the evidence is this raw and immature," ICER President Steven Pearson said in an interview with NPR. "But it was quite clear that the world is moving at a much quicker pace."
If the price is based just on the cost of making the drug, then a 10-day course of remdesivir should cost about $10, according to the ICER report. (Gilead said results of a recently completed study suggest a five-day course of treatment may be just as effective.)
But if the drug is priced based on the drug's effectiveness, ICER estimates it should cost around $4,500 — assuming the drug is proven to have some benefit on mortality. If it doesn't and the drug only shortens hospital stays, that value-based price goes down to $390.
Results from a federally funded study described by Anthony Fauci, director of the National Institute for Allergy and Infectious Diseases, suggested that remdesvir could reduce recovery time by a median of four days — 11 days to recovery for patients treated with remdesivir compared with 15 days for those who got a placebo. A potential survival benefit is less clear.
Rutgers's Carrier said he expects Gilead to set the remdesivir price somewhere between the $10 and $4,500 that ICER estimated. The company has already shown that it can respond to public pressure when it asked the FDA to rescind the orphan drug status it won for remdesivir, he pointed out.
"When you see that $10 figure, that sets a benchmark for a figure that is eminently affordable," Carrier said. Ultimately, he said a price more than $1,000 per treatment course would be unpopular.
Gilead "will be watched very carefully," he said, because of its prior history of pricing. He referred to two other Gilead drugs that drew scrutiny over high price tags. The company charged $1,000 per pill for Sovaldi, a cure for hepatitis C. And its HIV drug Truvada can cost $22,000 per year.
But there is such a thing as pricing remdesivir too low, said Craig Garthwaite, who directs the health care program at Northwestern University's Kellogg School of Management.
"We don't think this is the only drug we need," he said, adding that remdesivir doesn't appear to be a "home run" against the coronavirus, based on existing data. "The thing that would worry me the most is that we're somehow telling people that if you take the risky bet to try, and you'll go after a coronavirus cure and you do it, you're not going to get paid."
Instead, he said he would like to see acceptance of a generous price for remdesivir to send the message to drug companies that the best thing they can do is "dedicate every waking moment to trying to develop that cure, and that if they do that, we will pay them the value they create," he said.
During a Gilead earnings call on April 30, analysts asked executives whether they could expect similar financial returns on remdesivir as they've seen with Gilead's other drugs.
"There is no rulebook out there, other than that we need to be very thoughtful about how we can make sure we provide access of our medicines to patients around the globe," Gilead CEO O'Day said. "And do that in a sustainable way for the company, for ... shareholders, and we acknowledge that."
On May 1, the FDA authorized remdesivir for emergency use, meaning it will be easier to administer to hospitalized patients with severe disease during the pandemic, but the drug is not yet officially approved. The federal government is coordinating distribution of the treatment.
Day acknowledged on the recent earnings call that the company "could" charge for remdesivir under an emergency use authorization, but he stressed that Gilead is donating its current supply, which should last through "early summer."
To date, the National Institutes of Health said it has obligated $23 million toward its COVID-19 remdesivir trial. And the U.S. Army Medical Research Institute of Infectious Diseases did some of the early in vitro and animal studies with the medicine prior to the pandemic.
"Taxpayers are often the angel investors in pharmaceutical research and development, yet this is not reflected in the prices they pay," Reps. Lloyd Doggett, D-Texas, and Rosa DeLauro, D-Conn., wrote in a April 30 letter to Health and Human Services Secretary Alex Azar.
Concerned about remdesivir's price, they asked for a full breakdown of taxpayer funds that have gone toward the development of the medicine. "An unaffordable drug is completely ineffective," they wrote in the letter. "The substantial taxpayer investments in COVID-19 pharmaceutical research must be recognized." [Copyright 2020 NPR]



