For Cancer Patients, Anguish Grows Over Deferred Surgery As Risk Rises
Last June, days after her 40th birthday, Silver felt a lump in her left breast that turned out to be a tumor that had spread to her lung and liver.
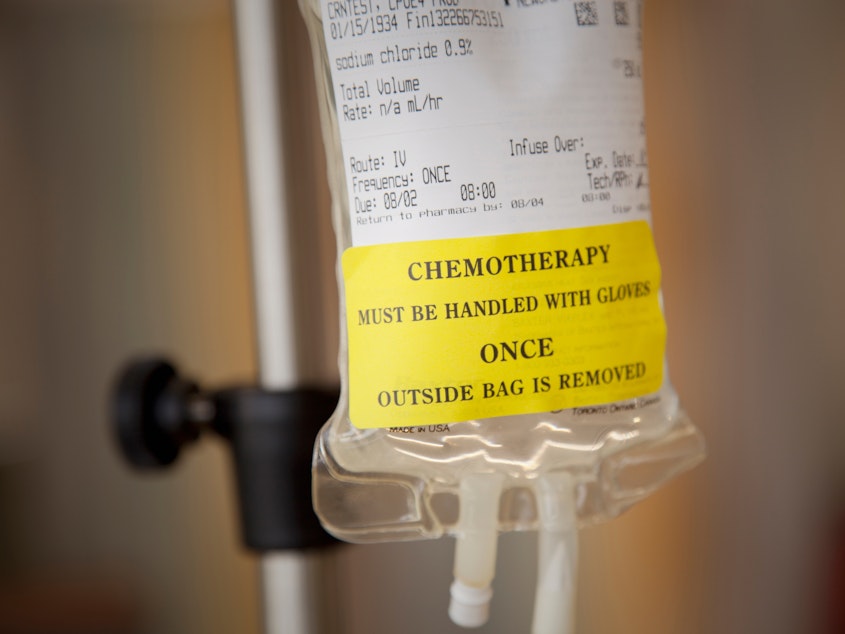
For eight months, she underwent chemotherapy that reduced the masses to operable size. But last month, Silver's oncologist explained a mastectomy would also require an additional procedure to take skin off her back, known as a "flap" to cover the wound.
That secondary surgery was considered cosmetic and therefore nonessential, according to the standards put in place this spring because of the coronavirus pandemic. Silver's surgery, like many others, was put on hold.
"It's not necessarily considered a medical emergency by them, even though it's, like, the entire world to me," Silver says. NPR is using only her first name, at her request, to preserve her medical privacy.
She felt shattered, she says, especially because she was unable to see her parents or get hugs from her friends.
"My one hope to be a long-term survivor was kind of fading, and now I'm going to have to pioneer a new hope," she says. "That was tough. It was awful."
COVID-19 has taken the medical focus away from many other serious diseases, including cancer. According to the American Cancer Society, more than a quarter of patients with active cancer are reporting delays in treatment. Also, cancer screenings are down, meaning many conditions will worsen while the health system diverts to fight the virus. At the same time, the pandemic is creating bottlenecks in care.
"We are paying a price with lives lost — not only from COVID-19 — but from people who need medical care and are afraid to get it or reluctant to go," says Len Lichtenfeld, deputy chief medical officer of the American Cancer Society in Atlanta. He says his organization's study on disruptions to cancer care from hurricanes shows that sort of missed care has an impact on survival rates, for example — and the pandemic is stretching out over a much longer period of time than a hurricane.
"We've always said we have to do everything immediately in cancer care," but oncologists and patients are having to wait or start other treatments instead as they wait for surgery.
For Silver, such delays are excruciating. Her oncologist suggested a new chemo until surgery is possible. But to change the chemo, she needed to get another biopsy, the doctor told her. And then there was a delay in getting that second biopsy because there were few members of the staff available during the pandemic to do it.
And that's not all: Insurance approvals take longer now that many agents are working from home, she says. And the chemo center takes fewer patients throughout the day to space the treatment chairs farther apart. The time each delay steals is precious.
"In the five-week delay, I had gone from three small tumors to a massive, 7- by 3-[centimeter] tumor that was pushing against the skin," Silver says, fighting emotion.
This heartbreaking scenario could play out for many people.
"We're only going to realize over the next few months and years about what the consequences of that deferred therapy are," says Ravi Parikh, an oncologist at the University of Pennsylvania. He says recent months forced him to embrace the previously unthinkable — including in-home chemotherapy and patient visits conducted over the phone. Such workarounds, he says, will need to continue.
"The No. 1 thing that I'm concerned about is the backlog of cases," Parikh says. "When there's this onslaught of appointments, surgeries, colonoscopies, chemotherapy appointments, it's not going to be at a slow pace."
Nor will it be able to happen quickly. Cancer patients with weakened immune systems are at greater risk of infection — and that risk continues, even as states start to reopen. Their risk varies by community even within a region, so doctors will have to weigh when it's safe to operate in their local area. And as they resume widespread treatment, each doctor, medical practice or treatment center will face the challenge of determining who receives care first.
The University of Michigan's hospital system is already using a new formula as those decisions arise about who should get priority in treatment — to include factors such as the nature of the disease and its progression, says Michael Sabel, a surgical oncologist and professor. Patients are assigned what the hospital calls an "urgency score," Sabel says.
"In many cases, that can include patients being able to get back to work, and the financial strain that's on patients — in addition to just things like, is it cancer and what is the biology of that cancer," he says.
Still, the frustrating reality is that COVID-19 will continue delaying care for some time.
Silver has set her sights on new goals: to shrink the tumors with the new chemo and to reschedule surgery for the fall.
"I hope it works," she says. "It's what I have right now — and I just hope it works." [Copyright 2020 NPR]



