A year in, experts assess Biden's hits and misses on handling the pandemic
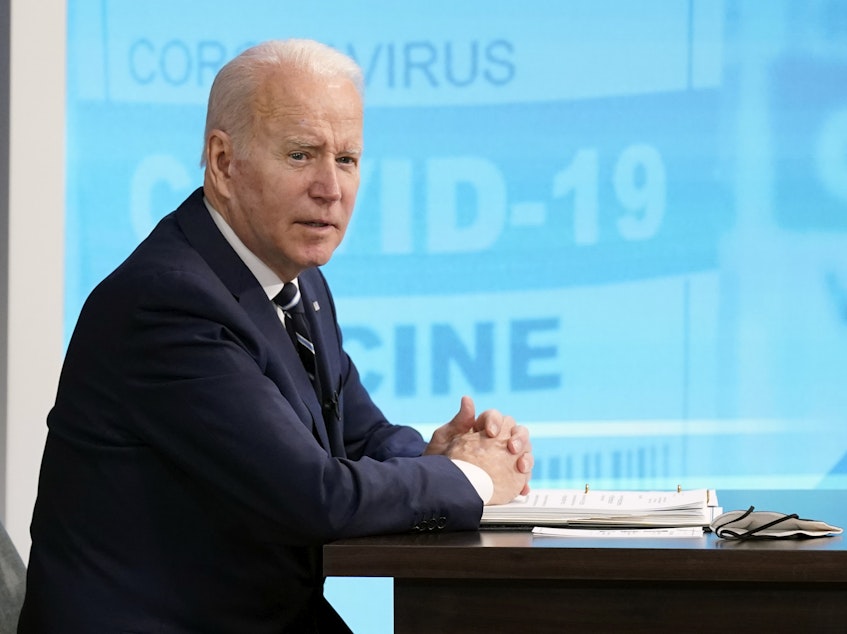
Last January, 2021, the day after he was inaugurated, President Biden released a national strategy for beating COVID-19. The 200-page document was hailed as "encouraging" and "well-constructed" – a pandemic exit blueprint that had not been articulated by the Trump administration before it.
"The plan itself is well-articulated, clear and ambitious – appropriate given the challenge," says Michelle Williams, an epidemiologist and dean of the Harvard T.H. Chan School of Public Health. But, she adds, "execution is always challenging."
At the time President Biden assumed office, cases and deaths were hitting record highs and the newly launched vaccines were in short supply. To move the country past "a dark winter of this pandemic," Biden pledged to restore public trust, vaccinate the country, minimize COVID-19 spread and reopen society – with a focus on equity – and resume America's global leadership.
The effort "started off really well," says Dr. Georges Benjamin, executive director of the American Public Health Association, "The challenge is that this virus continues to throw us curves."
Reality set in as states and employers filled gaps in communication and coordination with wildly varying policies. The public lost its appetite for new guidance as pandemic fatigue increased. Then came the delta variant. And omicron. And yet another winter with new cases hitting new record highs.
One year after the release of Biden's initial National Strategy for the COVID-19 Response, NPR spoke with experts in health law, epidemiology, virology and more to evaluate how the administration performed on the President's seven pandemic goals – and what lessons to take as the country moves through this public health crisis.
Goal 1: Restore trust with the American people
Trust is key in a pandemic – if the public doesn't trust what the government says, they're unlikely to comply with public health recommendations.
America was already deeply polarized and distrustful of government before the pandemic. Then, under the Trump administration, political interference, incomplete information, and confusing messaging further undermined public trust.
Experts say on this front, the Biden administration has not made much progress, although they acknowledge how challenging a problem it is. Public trust in government has improved slightly, compared with 2020, but it hovers at historic lows. And only about 50% of Americans recently said they trust public health institutions like CDC and state health departments.
"It's very difficult to rebuild trust once it's been lost," says Lindsay Wiley, a health law professor at UCLA. "Restoring trust is a lot harder than maintaining it in the first place."
The Biden administration pledged to let scientists and public health experts drive its COVID strategy. Benjamin says the commitment alone has transformed the tone and perception of the government response.
"We don't have [White House officials] trying to edit the [CDC's publications] or going onto the CDC's website and changing what's there," he says, referencing moves by the Trump administration. "We have some growing pains around communication, but those are bumps in the road and honest errors."
But recent missteps by the Centers for Disease Control and Prevention and continued communication problems have reinforced a public perception that the administration's guidance is "utterly chaotic," says Wiley. "It has seemed reactive, instead of proactive, and it's changed in ways that haven't been clearly explained."
Health experts say these are unforced errors. The CDC must be more clear and transparent about what science exists, and how it informs their decision making – or risk further tanking public trust.
Goal 2: Mount a safe, effective, comprehensive vaccination campaign
President Biden inherited a nascent COVID-19 vaccination program with severe supply constraints. His administration made huge strides in expanding vaccine supply and access, experts say.
"This is the jewel in the crown of the plan," says Michael Fraser, CEO of the Association of State and Territorial Health Officials. The unprecedented coordination between federal, state, local health authorities and pharmacy partners, he says, resulted in 500 million COVID-19 vaccine doses administered in Biden's first year in office; 75% of the U.S. population now has at least one dose.
Still, "that expanded access has not been met by the acceptance of the vaccine," says Williams. Over 60 million people in the U.S. eligible for shots remain unvaccinated, and the Administration has had little traction in swaying them. "The administration still has a huge challenge in addressing those that are resistant and hesitant of vaccines."
Those who remain unvaccinated are largely Republicans who oppose the Democratic President. There's also lagging vaccine uptake among rural residents, younger adults, and children. Vaccine disinformation fuels intransigence.
"It's going to require increased effort and elevated capacity to speak in meaningful ways to the hesitant, the concerned and the resistant populations," says Williams.
Continued investment in researching and developing new COVID vaccines is also needed, Fraser says: "We can't rest on our laurels here." Vaccines that work against current and future variants, or are easier to make, distribute and administer are critical for staying ahead of an evolving virus.
Goal 3: Mitigate spread through expanding masking, testing, treatment, data, workforce, and clear public health standards
This is an area where the administration has fallen short, says Seema Lakdawala, a virologist at the University of Pittsburgh who's been tracking the impact of COVID-19 mitigation measures. She says this is an area of "missed opportunities" for the administration.
"I do think that there may have been an overemphasis on vaccination as being the easy way to solve this at the cost of testing and other mitigation strategies that we could have continued to do to reduce some of the burden that we've seen," Lakdawala says.
The pandemic is a complex problem that requires a multi-faceted response, says Williams. "There is a human tendency to reduce it down to the one magic bullet," says Williams. "But the thing that's most humbling about this pandemic is there is no one magic trick."
The White House is now putting more muscle into these other strategies for curbing spread. It plans to begin distributing one billion free rapid COVID-19 tests starting Wednesday, and also make "high-quality" masks available for free.
Still, the government has seemed to waffle on the importance of tests and masks. For instance, CDC has not encouraged states to bring back mask mandates during the omicron surge, and has resisted calls by experts to add a negative rapid test before returning to work to its quarantine guidelines.
As much as the administration may have aspired to create and execute a national approach to these mitigation tools, it has come up against the decentralized U.S. public health system, says Fraser, in which states and counties can largely do their own thing. "We do have inconsistent masking guidance, we do have inconsistent access to testing, we do have inconsistent treatment or therapeutic availability because there's scarce supply and states are getting different amounts – that's the system we have," he says.
"I think that they did what they could – in federal buildings, on airplanes and airports and trains and buses – but, by and large, these mitigation efforts are designed so states can protect their residents," he adds. The result is a confusing patchwork of policies.
Goal 4: Immediately expand emergency relief and exercise the Defense Production Act
The President scored an early win signing the American Rescue Plan into law in March. The $1.9 trillion package included direct payments to individuals, an extension of federal unemployment benefits, a temporary child tax credit, another round of small business loans, and more. Nearly a year later, most of the benefits targeted to families and individuals have expired.
As for the Defense Production Act, which the government can use in times of national emergency to get companies to prioritize their medical supply contracts, attorney Franklin Turner, a partner and co-chair of the Government Contracts and Global Trade Practice Group at the law firm McCarter and English, says he thinks "this administration in particular has been quite skillful with respect to its use of the DPA." That's despite widespread frustrations that COVID-19 tests and high quality masks have often been hard to find in many places.
An analysis from the Government Accountability Office last month found that the government used its authority "over 100 times to help address COVID-19 medical supply needs through September 2021."
Still, "the main message here is too little, too late on masks and testing," says Wiley. In the current omicron surge, the nation's testing capacity has been severely crunched. As for quality masks, such as N95's and other high-filtration respirators, "it's kind of a Wild West market," she says, "There are counterfeits everywhere." From Wiley's perspective, the administration has made inadequate use of their supply chain authority, and their guidance to the public on how to procure and make the best use of masks and tests has been lacking.
From Turner's perspective, the current supply problems have less to do with underutilized federal authority and more to do with the virus itself. "Just because a supplier receives a sheet of paper that says produce, for example, 100 million N95 masks, folks have to be able to show up to work to make those, you have to be able to ship them," he says. "The virus has just been so bad that folks have been increasingly unable to keep up with the pace of demand."
Goal 5: Safely reopen schools, businesses, and travel, while protecting workers
Schools continue to be a contentious issue – with recent student walkouts, teachers' union strikes, and public health experts fiercely disagreeing about what's safest and best for kids at this moment. Even so, most schools across the country have been able to stay open even as cases have spiked.
Dr. Luciana Borio, a senior fellow for global health at the Council on Foreign Relations counts that as a success. For the most part, she says, "schools and businesses remained open even during the last surge with omicron, and that's not a small feat."
The country's decentralized structure has made it difficult to achieve uniformity, says Fraser. "Local systems and schools are making decisions in their township or their county," he says. "There's no way the feds can control what that looks like locally."
There are certainly business closures and worker shortages, but those seem to be more due to omicron than federal policy. The federal government recently shortened its quarantine and isolation recommendations in an effort to help with worker shortages and "keep society running," as CDC Director Rochelle Walensky told NPR.
Another aspect of the administration's plan – protecting workers through a vaccine mandate – took a major hit last week with the Supreme Court blocking the White House's attempt to require vaccination or tests for employers with 100 or more workers.
Goal 6: Protect those most at risk and advance equity, including across racial, ethnic and rural/urban lines
The administration has been "moderately successful" on this front, says Benjamin of the APHA. Biden convened a COVID-19 Health Equity Task Force, to address pandemic-related health inequities. Earlier in the pandemic, rates of infections and deaths were higher in communities of color and low-resource communities, many of whom had less access to health care to begin with, and were less able to adapt their living and work situations to reduce COVID-19 exposures.
Gaps in vaccination and death rates between the majority white population and communities of color have greatly narrowed or closed. These numbers represent significant investment from the federal government and hard work focused on equity, says Fraser. "It was an all-hands-on-deck, block-by-block kind of campaign, and it still continues," he says. "There's [still] a tremendous amount of work to do here, especially in building trust in communities of color, but it's not for lack of trying."
But masks and tests are still expensive for many people, says Williams. "It's unconscionable that low-income families, up to now, have had to pay $12 to $20 for [at-home rapid] testing," she says, "High-quality masks and access to rapid testing has to be the next major initiative where equity lens is brought forward."
President Biden has announced plans to make masks and take-at-home COVID-19 tests free to the public – and his administration issued a rule requiring private insurance plans to cover the tests. Beyond addressing acute shortages, the Health Equity Task Force's final report made several dozen recommendations to mitigate health disparities caused by this pandemic, and to help course-correct an inequitable health system going forward.
Goal 7: Restore U.S. leadership globally and build better preparedness for future threats.
Biden moved quickly after he was inaugurated to rejoin the World Health Organization, which Trump had pulled out of – and provide some leadership within global COVID forums, says Benjamin. "I think there's still some work to be done, but I do think that they've really jumped in with both feet," he says.
Biden pledged to donate over a billion vaccine doses to countries around the world. Federal officials point out this is more than all other countries combined.
But critics say it's still not enough and not fast enough. So far, the U.S. has only delivered about 330 million of those doses. As the emergence of omicron illustrates, the more of the world's population is unvaccinated, the easier it will be for the virus to mutate and continue to cause new waves of infection domestically.
"We clearly have not vaccinated the world," says Dr. Celine Gounder, an infectious disease physician and epidemiologist at NYU. "We have missed multiple deadlines set by the WHO for vaccination targets, and their newest vaccination target we will probably miss as well."
Part of the problem, she says, has been an apparent resistance to help other regions of the world manufacture Pfizer and Moderna's COVID-19 vaccines for themselves. "The U.S. government owns the patent on some of the technology in the Moderna vaccine and has not used that lever to force sharing of technology and manufacturing know-how with others to allow for that kind of scale-up."
This "is certainly an area where the administration promised big but has fallen short so far," she adds.
And the U.S. could have done more, says Borio of the Council on Foreign Relations. "We're uniquely positioned to help do that given our historical role and also the fact that our science is incredible and that we have these amazing, safe and effective vaccines."
The goal also mentions preparing for future threats – that is also an area that needs work, says Borio. "That is something I really worry very much about – biological threats continue to represent a grave threat to national security and to our health security," she says.
Even with the omicron surge, she adds, "we can't just say, 'I'm going to deal with this later because I'm busy right now.' " There's no guarantee the country will have a quiet moment to regroup, she says, before the next threat strikes. [Copyright 2022 NPR]



