How Herd Immunity Works — And What Stands In Its Way
What will it take to finally halt the spread of the coronavirus in the U.S.? To answer that question we've created a simulation of a mock disease we're calling SIMVID-19.
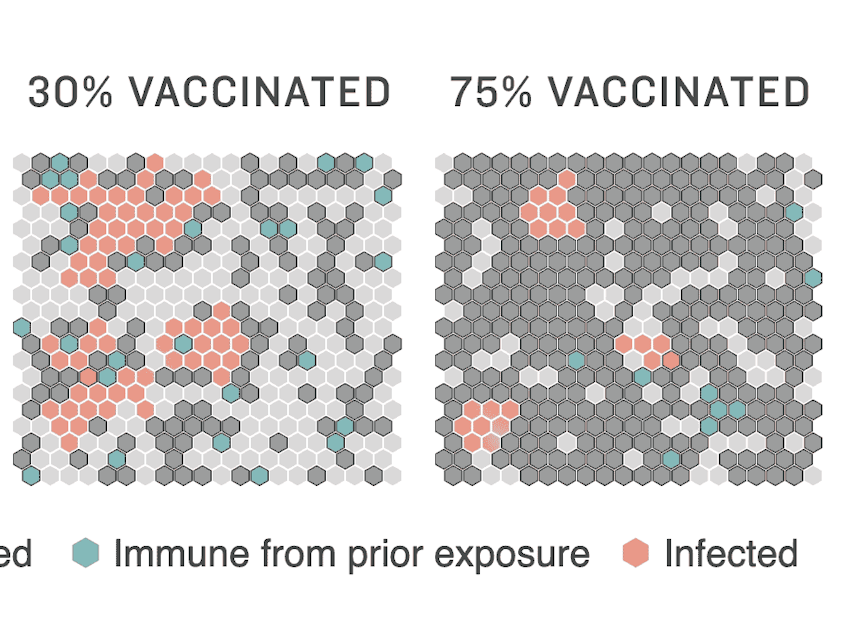
When you click "Run Simulation" above, you are witnessing how a disease can spread through a population and how increased levels of vaccination can stop it in its tracks.
We're chosen to simulate a fake disease since there are too many unknowns to simulate the course of COVID-19. There are common features in how any infection spreads. When enough people are immune — through vaccination or natural immunity — a population achieves herd immunity. The disease stops spreading efficiently and starts to fade away.
How quickly a community gets to herd immunity depends on a number of factors. We've illustrated some major ones in the scenarios that follow.
1) A more infectious variant takes over
Sponsored
What happens if a more infectious strain of SIMVID-19 predominates in a community? You can see in the simulation that even at a 75% vaccination rate, many people in our imaginary community of 400 will still get infected.
It looks like it will take higher vaccination rates to achieve herd immunity against the more infectious strain of SIMVID-19. This is a real concern with emerging variants of the coronavirus, including the strain first detected in the U.K., which is now spreading rapidly in the U.S.
There's always an element of chance in how diseases spread, as you can see each time you re-run these simulations.
2) A population is already heavily exposed
The pandemic has hit some communities harder than others, leaving in its wake some degree of natural immunity. This scenario assumes a lot of people are already immune to SIMVID-19, through a previous infection.
Sponsored
For this illustration, we've decided that a SIMVID-19 infection will persist for the duration of our simulation. You can see how higher levels of immunity — along with a high vaccination rate — would help a community reach herd immunity. For the coronavirus, we don't know what percentage of people who have been infected are immune, or how long that immunity lasts.
3) A population has low levels of initial immunity
You can see in this scenario how SIMVID-19 can spread more easily in a population where few people are immune at the start of an outbreak. It is harder to achieve herd immunity in this scenario, and increased levels of vaccination are key. When it comes to coronavirus, some communities have lower level of preexisting immunity and scientists think that the immunity people do have may fade over time.
Takeaways for COVID-19
In our SIMVID-19 scenarios, 75% vaccination rates were able to kick the imaginary disease in all but one scenario, the more infectious variant. For the U.S. to tame its coronavirus outbreak through herd immunity, scientists expect that somewhere between 70% and 85% of the population must be immune.
Sponsored
Unfortunately, we can't predict exactly what vaccination rate will be needed because there are many questions about the coronavirus we simply can't answer.
For example, people who are vaccinated may still pose some risk of spreading the virus, even though the vaccines protect them from serious illness. And no vaccine is 100% effective, so some vaccinated people will still get ill and could still pass on the disease. You can see this in our model, as dark-gray, vaccinated individuals turn infected pink, from time to time.
And though we do know that perhaps 120 million Americans have already been infected, we don't know how long immunity following infection will last. Finally, there is a concern that some variants now spreading around the world will render vaccines less effective.
One thing that's evident from this simulation (and real life) is that the faster the population is protected by vaccination the better.
Methodology
Sponsored
Our simulation of SIMVID-19 simplifies a lot of the details of how diseases like the novel coronavirus spread for illustration purposes. For example, each cell in our hexagon grid only has a maximum of six other "people" that it comes in contact with, and there's a fixed chance that an infection will spread from one cell to another. Vaccination reduces that chance, but doesn't eliminate completely (as is true in real life). That means that if you re-run the simulations over and over, you may get a lucky or unlucky roll from time to time. To keep these outliers from creating confusion, the first simulation run in each scenario starts from an identical configuration.
Daniel Wood and Carmel Wroth contributed to this report. [Copyright 2021 NPR]


